On 12 October 2024, the SMA Centre for Medical Ethics and Professionalism organised a webinar titled "Ethical Analysis in Decision Making for Patients with Diminished Capacity".
The clinical case discussed during the webinar was of a female patient with Down syndrome with moderate intellectual disability who had developmental dysplasia with secondary osteoarthritis and avascular necrosis of her right hip. This had severely limited her mobility and caused her considerable pain. The initial surgical consultation resulted in a conservative non-surgical rehabilitative approach. This approach did not relieve the pain, and the patient became bed-bound. A second surgical consultation was arranged with the senior surgeon who was experienced in caring for patients with intellectual disability (PwlDs). Surgical intervention was offered, which the patient's family accepted. The surgery and subsequent post-operative rehabilitation resulted in good functional recovery and pain relief. Her family was actively involved, and the patient was supported by the team from the Movement for the Intellectually Disabled of Singapore clinic.
We explore in this article the ethical analysis and relevant discussions based on the above case scenario.
What is ethical analysis in clinical practice?
Ethical analysis involves identifying the problem, gathering the relevant information, evaluating the options and making a decision. In practice, it involves a systematic approach to applying ethical theories and principles to the clinical situation. It therefore connects theory to practice by using critical reasoning to arrive at a justifiable and defensible clinical decision.
Clinical ethics deals with ethical issues arising in the clinical care and treatment of patients and the practice of clinical medicine. Clinical ethics uses ethical reasoning to guide decision-making and thus achieves good patient outcomes and builds trust between the healthcare team, patients and their families. In clinical situations when the ethical position is unclear, ethical analysis helps to guide the clinician to arrive at what the right thing to do for the patient should be. It helps clinicians to appreciate why some options are acceptable and others unacceptable in that situation.
There are several methods available for clinical ethical analysis:
- Four-topic (or box) approach by Jonsen, Siegler and Winslade
- The four principles approach by Beauchamp and Childress
- Approach to ethical dilemmas in clinical medicine by Lo
- The five-step model by Veatch, Haddad and English
- Clinical ethical reasoning by Rhodes and Alfandre
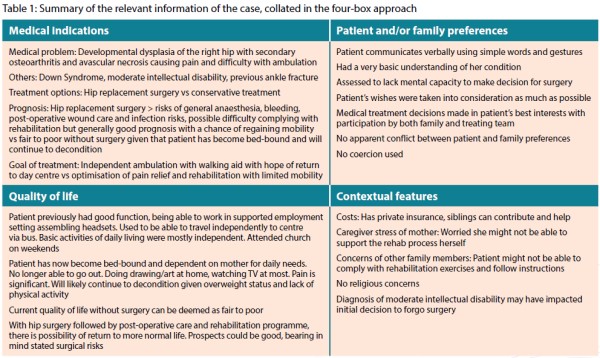
In this article, the four-box approach is used for the ethical analysis of the clinical case (see Table 1).
Ethical analysis using the four-box approach
This approach is familiar to clinicians and includes the orderly collection of data and its collation into four topics. Each topic links the clinical data and facts of the case to the ethical principles and helps bridge theory to practice.1
The approach involves the collection and collation of relevant information from the case, into the four topics:
- Medical indications (Principles of beneficence and non-maleficence)
- Patient and/or family preferences (Principle of respect for patient's autonomy)
- Quality of life (Principles of beneficence, non-maleficence and respect for patient's autonomy)
- Contextual features (Principle of justice, fairness and fidelity)
Medical facts and indications
The pain in the hip resulted in the patient becoming wheelchair/bed-bound and completely dependent on her caregivers for her daily activities. The recommended treatment was surgery with hip replacement to alleviate pain and allow for greater mobility. With regained mobility, the patient could be independent in most of her activities of daily living. There were no major medical contraindications to surgery, and no coexisting medical morbidities other than being overweight. The principle of beneficence is thus supported.
The main concern of the proposed surgical treatment was the patient's ability to follow instructions in the post¬operative rehabilitation. The concerns were of resulting poor wound healing and wound infection. Here, the principle of non-maleficence was considered.
While conservative management and active pain management may avoid the risks associated with surgery, it would not enable mobility or improve independence, which may result in significant caregiver stress and possibly residential nursing placement.
In summary, the patient would benefit from a hip replacement surgery for both pain relief and mobility. With patient-centred post-operative care, the risk of surgical complications could be minimised.
Patient and family preferences
The patient could communicate verbally using simple words and gestures. She did not have the mental capacity for medical decision-making for the surgery.
At the first consultation, the family declined surgery as they were informed of possible post-operative complications. The consequences of not having the surgery, and of persistent pain and immobility were not adequately discussed.
The family believed that the patient's quality of life would improve if she could be mobile and independent in her activities of daily living. In the long run, she could return to the work that she enjoyed at the sheltered employment centre. As the patient had diminished mental capacity all her life, there were no prior written discussions or advance medical directive. Using sign language, her expressed wishes and preferences were to be relieved of pain and to be mobile. The family worked with the medical team by applying the best interest principle in the decision-making process.
In summary, when given the full information on the therapeutic options and their consequences, the family was able to decide that the best interests for the patient was to undergo surgery. By applying the best-interests principle in decision-making, respect for the patient's wishes was upheld.
Quality of life issues
With surgery for hip replacement followed by post-operative care and rehabilitation, the prospects of returning to a good quality of life were assured with improvements in her physical, mental and social health. Caregiver burnout could also be averted.
In summary, the surgical approach provided for the best quality of life by enabling the patient to be mobile and pain free.
Contextual issues
There were no financial, religious or cultural issues with regard to decision-making with the patient and family. The other contextual issue was of the experience and expertise of the surgical team in working with a PwID in the peri-operative and rehabilitation stages.
In summary, as there were no resource limitations or conflict of interest issues, the ethical principles of distributive justice and non-discrimination are upheld.
Conclusion
In this ethical case analysis, the dilemma was related to the lack of full discussion on the consequences to the patient's well-being caused by the therapeutic options of hip replacement surgery versus conservative non-operative care. When given the full information and taking a shared decision-making approach, the family was empowered to decide that surgery was in the patient's best interests. Surgery and post-operative rehabilitation benefitted the patient and the family, by enabling the patient to be mobile and more independent, and preventing a deterioration in the patient's quality of life and her family experiencing caregiver burnout.
In the clinical care of patients with diminished mental capacity, healthcare professionals must take on the role of being health advocates for the patient for medical beneficence to be upheld. To be an effective health advocate, healthcare professionals need to have a good understanding of the patient's and family's perspectives of the illness and be innovative in assembling a team with experience and expertise to manage the medical issues of patients with diminished capacity.