Much has been said about how well Singapore's healthcare system has fared in dealing with COVID-19. Less talked about is how its junior doctors (including residents) in the restructured hospitals have shared much of the burden of holding up the country's healthcare system. Many of them have seen their relatively nascent careers disrupted by the pandemic in unexpected ways. Stress and burnout issues among junior doctors, while no doubt already existing pre-pandemic, were brought to the fore during the pandemic.
Impact of the pandemic on junior doctors
In the early days of the pandemic, many junior doctors were deployed to outbreak wards and community facilities to manage the burgeoning number of COVID-19 cases. Within the National Healthcare Group (NHG), residents willingly and unhesitatingly responded to the call to serve in the National Centre for Infectious Diseases (NCID) and in other outbreak response roles. Meeting rooms were transformed into war rooms where outbreak response strategies were discussed. ICU-trained junior doctors turned into frontline soldiers. It was an exceptional time - a time when many readily placed national and institutional needs over their own. All hands were on deck.
But as the months wore on, fatigue set in. With annual and training leave frozen, overseas travel cancelled, and mandatory split team assignments in place, morale and emotional well-being took a hit. With safe-distancing measures in place, peer support – which would have developed organically pre-pandemic through conversations over post-round "kopitiam" breaks, lunches and watercooler breaks – were consigned to a distant memory. With reduced social interaction, work became more sterile, both in the literal and figurative senses of the word.
As doctors began isolating themselves out of fear that they would pass the virus to their loved ones, junior doctors were not spared. We once spotted a junior doctor sitting alone at the link bridge between the NCID and Tan Tock Seng Hospital (TTSH) buildings, worrying over whether to go home or to stay on in the hospital. Dealing with morbidities and mortalities from COVID-19 was emotionally draining for junior doctors. Yet, with the sheer volume of cases relentlessly flooding the hospitals on a daily basis, there was little time and space to pause and rest from the many heart-breaking moments from a typical day at work.
There was also increased anxiety over career trajectories. The deployment of junior doctors to areas outside of their specialty requirements, coupled with restrictions on staff movement and split-team assignments, inevitably resulted in disruptions and interruptions to training and teaching programmes. In an effort to prioritise resources to the national crisis, didactic and clinic teachings were temporarily paused, and workshops and courses were halted. Residents found it challenging to obtain the usual variety of clinical exposure and fulfil the number of procedures, especially elective ones, required for their respective training programmes. Post-graduate professional examinations, exit examinations and their associated preparatory courses were also cancelled or postponed, occasionally at the eleventh hour.
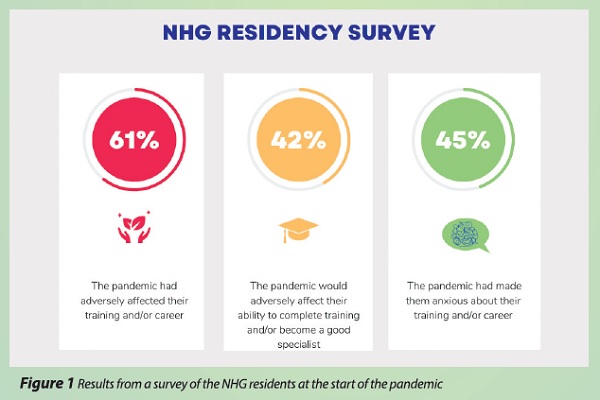
In a survey of NHG residents conducted at the start of the pandemic, 61% of the respondents agreed that the pandemic had adversely affected their training and/ or career, 42% agreed that the pandemic would adversely affect their ability to complete training and/or become a good specialist, and 45% agreed that the pandemic had made them anxious about their training and/or career.1 These numbers speak for themselves.
With this new normal, it became clear that action was needed - not only to protect the welfare of junior doctors, but also to enhance their capacity for growth and resilience so that they would survive this pandemic and emerge from it stronger. Within NHG, senior doctors who had fought through and survived the SARS outbreak in 2003 stepped up to provide insight from their own experiences and became an essential source of encouragement to our junior doctors. Cluster-wide initiatives were introduced, and their successful implementation was made possible only with strong and unyielding support from the NHG leadership team.
NHG's initiatives
The NHG Residents' Council, which is a part of the NHG Graduate Medical Education Committee, comprises chief residents across all the residency programmes. A key role of the Residents' Council is to engage with NHG residents and address their feedback and concerns.
During the pandemic, the Residents' Council maintained channels of open communication between NHG residents and NHG senior management through organising regular dialogue, gathering feedback from the residents, and channelling this feedback to the senior management. At the height of the pandemic, when healthcare protocols were in a constant state of flux and concerns over them were abounding, the Residents' Council sought to facilitate prompt and effective communication by regularly engaging with the chairmen of the medical boards of the respective NHG hospitals and the NHG CEO.
Events to boost the morale of junior doctors were also organised - the "NHG Most Valuable Player Awards" campaign sought to honour junior doctors who have displayed outstanding character, and food and drink treats were distributed across the year (think Famous Amos cookies for Valentines' Day, Ya Kun Kaya Toast vouchers for Labour Day, and bubble tea for Bubble Tea Day because bubble tea deserves its own special day). It was heartening to see that some senior doctors in NHG even started a COVID-19 welfare fund to contribute towards funding these events.
The NHG Residency Wellness Committee also complemented these initiatives with their own. The Wellness Committee, which comprises representatives from the Residents' Council and NHG Residency faculty members, constantly looked out for the welfare of the NHG residents and junior doctors during the pandemic. A conscious effort was made to acknowledge their hard work and sacrifices, and to encourage them.
Initiatives that the Wellness Committee rolled out included creating a Burnout Assessment Checklist, introducing the SOAR (managing Self, Others, And building Resilience) framework, partnering with organisations such as Brahm Centre to provide counselling support, and leveraging on the TTSH Hospital Conference as a platform to address burnout and resilience among healthcare staff.
Rethinking stress and burnout
Stress and burnout among junior doctors existed pre-pandemic and will continue to exist post-pandemic. They are perhaps unavoidable, given the high-stress environment of the public healthcare system and the demands of the work of physicians. However, what the pandemic has provided is an opportunity for NHG to re-think how to make work for junior doctors more efficient. The key is to consider how to better protect junior doctors' welfare without compromising clinical care. As a start, discussions are underway with Ministry of Health Holdings to pilot 24-hour calls for NHG residents, in contrast to the current standard of at least 30-hour calls where residents have to continue with other work duties post-call. The pandemic has also highlighted the importance of establishing a culture of peer support, care and concern among junior doctors, where looking out for a peer in distress is not the exception but the norm, and where every small interaction with fellow colleagues and healthcare workers is encouraged, cherished and not taken for granted.
The work of the Residents' Council and the Wellness Committee in response to pandemic-induced stress and burnout is just a start. More can be done. More will need to be done as the demands on the healthcare system evolve. As we continue to serve our junior doctors and residents, we are cognisant that many big, complex, and seemingly insurmountable problems need not be resolved by mind-blowing revolutions, but by consistent and constant accumulation of day-to-day actions, both at the institutional and individual level.
Some of these actions include making sure lines of communication and feedback remain accessible and effective. Investing in our junior doctors not only through programmes that ensure proficiency in clinical skills, but also via platforms that focus on personal well-being. Showing concern to our peers by asking after them as we bump into them along the corridors. Lending a listening ear and providing a safe space over a cup of coffee. Offering help to a peer who is unable to cope with the demands of work. Extending kindness to someone who has had a long, hard day. Each small gesture can go a long way. We do not need to wait for systemic and policy changes to be implemented before being a source of encouragement and comfort to one another.
It is also worth remembering that while the practice of medicine and residency training has seen dramatic changes in recent years, the timeless values by which we carry ourselves as a profession remain constant. Ultimately, it is the sense of meaning and purpose in our calling as doctors that will see us through the difficult seasons - it is the COVID-19 pandemic today, it could be another healthcare crisis tomorrow. Viktor Frankel, the author of Man's Search for Meaning, puts it eloquently: "Those who have a 'why' to live, can bear with almost any 'how'." Hold tight to the convictions that drove you to pursue medicine; hold fast to the dreams and visions that you have for the medical profession. Remember them as you start each workday before the sun rises. Remember them as you chug your third cup of coffee for the day. Remember them as you feel yourself reaching your limit. The difficult seasons will pass, and it will all be worth it.
Acknowledgements
The authors would like to thank NHG's Designated Institutional Official Dr Faith Chia for her guidance and inputs in the writing of this article, as well as her continued support for junior doctors in NHG.
