Ms A, a 40-year-old lady, consulted me for a second opinion about an abdominal pain that had lasted for two years. She had previously been consulting another gastroenterologist, who did a gastroscopy and colonoscopy two years ago. Both were normal. General laboratory tests and imaging studies were also normal. She was told that nothing serious was found, and was treated as a case of irritable bowel syndrome (IBS) with symptomatic treatment.
However, she was still symptomatic with intermittent abdominal cramps, despite the medications. She asked her gastroenterologist if she needed another colonoscopy. Her specialist reassured her that as she had IBS, another colonoscopy would be unnecessary until five years after the first scope.
Ms A was somehow still very worried about a missed diagnosis, as her symptoms did not improve despite trying different kinds of gastrointestinal medications over the last two months.
Seeking a second opinion
At Ms A's first visit, I went through all her reports. She requested for a repeat colonoscopy. I agreed with her gastroenterologist that her diagnosis was IBS, and that a repeat colonoscopy was not warranted. Instead, I talked to her about a fermentable oligosaccharides, disaccharides, monosaccharides and polyols diet and lifestyle modifications, and treated her with a different kind of IBS medication.
Ms A came for a review two weeks later. Her symptoms of abdominal cramps and pain did not resolve. She remained very worried that she had some serious illness in her colon, and insisted on having a repeat colonoscopy to exclude any new or missed lesions in her colon.
I was in a fix. Generally speaking, if a colonoscopy is normal, the next surveillance colonoscopy could be done in five to ten years' time. Exceptions are made for poor bowel preparation or an incomplete colonoscopy, which warrants a shorter wait.
Her previous gastroenterologist was a colleague and friend. He was professional in his work, and I believe her scope was done properly. A repeat colonoscopy may be deemed unnecessary, yet a polyp or lesion could have been missed. As a matter of fact, up to 20% of small polyps can be missed on a colonoscopy, and even for significant polyps that are larger than 1 cm, 2% to 6% could be missed by colonoscopy.
The reasons for missed polyps could be purely technical. Small polyps can be hidden behind colonic folds. But improperly performed colonoscopy, such as short withdrawal times, suboptimal bowel preparations, or inattention/distraction during the procedure could also be a reason.
Ms A was very convinced she had some lesions in her colon. If I declined to do the colonoscopy, she was likely to look for a third gastroenterologist for a repeat colonoscopy. Besides, it had been two years since her last colonoscopy, and it was possible that new polyps had formed in her colon. If indeed something new had developed and was discovered by a third gastroenterologist, I could be accused of being professionally negligent.
Also, according to the Modified Montgomery (MM) test, the patient has the final say in what treatment they will receive. In my opinion, the MM test can be a dangerous concept. Patients do not always choose what is best for themselves. Nevertheless, this is the rule that we have to comply with.
Eventually, I documented the indications, risks and potential harms of a repeat colonoscopy to Ms A, and she consented to the colonoscopy.
The repeat colonoscopy
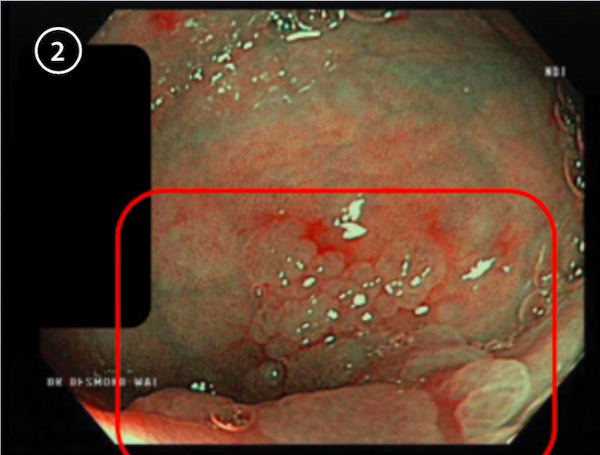
The procedure was performed with ease. But I found one 8 mm flat polyp around the cecum, as well as four polyps about 3 mm to 4 mm each in the rest of the colon. As a standard practice, I removed all polyps endoscopically. Fortunately, no malignancy was found on histology.
I broke the news to Ms A two days after her scope, when her histology results were available. I reassured her that she did not have colon cancer, and her symptom of intermittent abdominal cramps was due to IBS. I also showed her the endoscopic pictures, including before and after polypectomy photos (Figures 1 to 4).
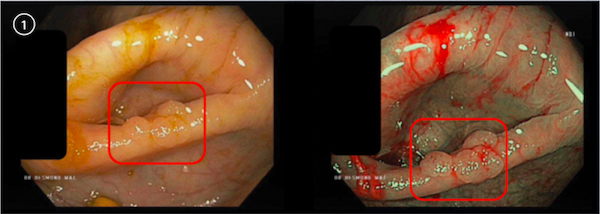
The flat polyp was identified within the red square
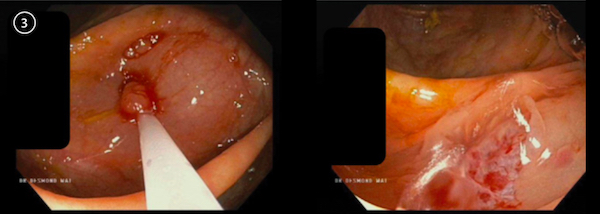
Polypectomy in progress
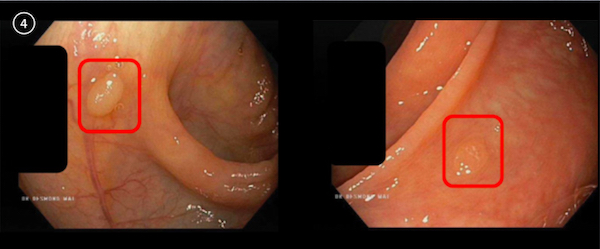
Another small polyp in the ascending colon
She was relieved that no cancer was discovered, but she was upset at her first gastroenterologist. She questioned why the 8 mm flat polyp was not found two years earlier, and was adamant that he refused to repeat her colonoscopy even though she had insisted. I spent some time explaining that the lesions could have been new, especially those small polyps found in her ascending and transverse colon. It was a bit difficult to explain the cecal polyp as it was big, but that could have been hidden by the colon fold.
She accepted my explanation and we decided to move on and focus on treating her symptoms. Before we finished, I asked her if I could have her permission to discuss her case with my friend, her first gastroenterologist. But she asked me not to, as she would not return to him.
I felt relieved that I repeated her scope and removed those polyps. We often face patients coming for a second opinion. Based on her persistent symptoms and normal up and down endoscopy two years ago, she would be labelled as a patient with IBS. But some patients, especially the more paranoid ones, would always worry that a diagnosis was missed, and request that tests (in this case a colonoscopy) be repeated. It is difficult for us on both ends. If we decline further tests, we save costs and risk for the patient. But if a serious diagnosis is found subsequently, we may be blamed for missing an opportunity for early diagnosis. On the other hand, we can just do what patients request. But if the findings are normal, then our procedure would be deemed unnecessary. Worse still, if complications arose from the procedure, like a postpolypectomy bleed or even a thrombophlebitis, then there will be medico-legal implications.
The risk of a colonoscopy is generally very low, with less than 0.1% resulting in serious complications. But in medicine, we can never say never. If indeed there was a complication arising from a scope that leads to a complaint or a lawsuit, the first thing that expert witnesses look at would be the indication.
Moving ahead
So how should we move on from here? Firstly, we need to do our jobs very seriously and professionally. For colonoscopy, optimal bowel preparation, adequate colonoscopy withdrawal time from cecum till anus, and keeping up-to-date with latest management guidelines and techniques are important. The first gastroenterologist did all these and I believe he would be fine even if Ms A lodges a complaint subsequently.
Secondly, we need proper documentation. Probability of a missed polyp and indications of a procedure, especially when they are weak as in Ms A's case, should be explained and documented.
Thirdly, we ought to be kind to our colleagues. If my colonoscopy for her turned out to be normal, and she consulted a third gastroenterologist, I hope he/she would be kind to me. If he/she accuses me of doing unnecessary scopes, then Ms A or her insurer may take legal action against me.
We all ought to give our colleagues the benefit of the doubt that we would not do unnecessary surgeries or procedures on patients. I am very sure some of my patients would consult other gastroenterologists for a second opinion. I cannot be 100% certain that every decision I make is right, and that I do every single scope without any complications. I just hope that we, in the medical profession, would be kind to one another when we discover insufficiency in our colleagues.