When I was first asked to help design and operationalise a mobile swab station (MSS) for COVID-19 in April 2020, I must admit that I was sceptical. After all, it had already been two months since our first local case, and our swab protocol seemed to be working just fine. Was there truly a need to kick up the dust or attempt to recreate the wheel?
As a junior Singapore Armed Forces (SAF) medical officer deployed to the migrant worker dormitories at that point, I remember feeling that there were far more important matters to deal with, and that this “side quest” was little more than a distraction. Three weeks later, my perspective turned a full 180 degrees (or as my encik would say, “kebelakang pusing!”).
As the swab requirements rose, there was an impetus to find a safe and efficient way to conduct these swab tests, particularly for non-purpose-built dormitories, which had no dedicated medical facility setup. Other challenges included a difficult terrain to navigate, paucity of permanent infrastructural facilities, and multiple dormitories requiring urgent swabs in a given day. Hence, the SAF designed the MSS as a “onestop swab shop” to tackle these issues.
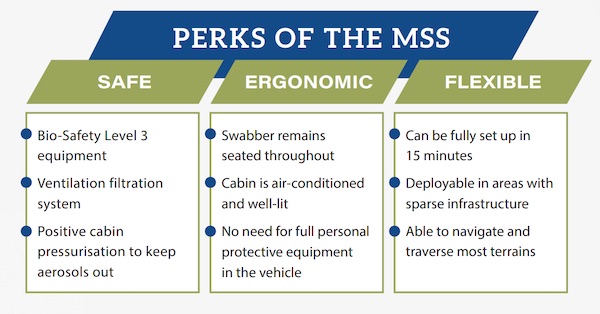
The MSS is an enclosed swab station integrated into our military vehicles. The MSS is designed to enhance safety, flexibility and efficiency in swab operations. With the healthcare workers inside the MSS to perform swab testing while the patients remain outside at the rear, this eliminates the need for healthcare workers to be in full protective gear throughout the swab operation. It was a fast-paced, operationally driven initiative, transforming from concept to capability in a short span of three weeks, compared to the usual threemonth duration.
Lessons learnt from the MSS design journey
Looking back, many of the lessons I learnt were applicable to clinical practice and, indeed, life in general.
The devil is always in the smallest details
One of the main challenges we faced was formulating a structural and protocolar design that prevented COVID-19 transmission from one patient to the next. With its big flappy arm gloves and multiple touch points, it was conceivable that the MSS could become just a really big fomite and we dove deep into the tactical details to ensure that this did not happen. We spent hours and days debating the design of the swab dispensing chute, reviewing multiple prototypes before picking one that balanced utility and ease of cleaning. We also surveyed medical literature and consulted infectious disease and public health experts to ensure that we adopted a robust disinfection process between patients.
Similarly, in conventional civilian clinical settings, the details matter. I have come across puzzling comments and instructions documented in patients’ records; eg, “patient refused medications” for a comatose patient, and “feast from 12 midnight” (instead of “fast from 12 midnight”) for a patient undergoing surgery the following day. More recently, a colleague shared that a full work-up for neutropenic sepsis was nearly performed for a febrile patient before somebody realised that the white blood cell count was 8.1, not 0.81. Good attention to detail results in safer medical practices and more favourable outcomes for our patients.
Everyone brings something to the table
The team that designed the MSS was cobbled together overnight and comprised representatives across the ops/technology spectrum. I played a relatively minor role in providing medical and force health protection input, engaging and functioning as the “medical translator” for various stakeholders, and conducting platform familiarisation training for swab teams. While COVID-19 is a major public health issue, this project was primarily the brainchild of civilian and military engineers. They oversaw the entire project, including air flow and filtration, materials and prototyping, funding and fleet expansion, and integration into existing SAF platforms. With input from HQ and ground teams, we sought to create a product that met everyone’s needs.
As healthcare workers, we are no strangers to team-based environments. From the medical student to the emeritus senior consultant mentor, to the cleaning auntie on the ward, everyone has an important role to play in the team, even if it is “just” drawing the curtains (with the requisite hand hygiene before and after touching them). I recall a story of a patient who was wheeled into the emergency department of a restructured hospital following a head injury and was nearly put on a mechanical ventilator for a low Glasgow Coma Scale (GCS) level. (As the saying goes, “GCS 8, intubate.”) Thankfully, a nursing student promptly pointed out that the patient was uttering phrases in Laotian, and were not “incomprehensible sounds” as perceived by the rest of the team, thereby raising his GCS level and sparing him a trip to the intensive care unit. Teams work best when members cover each other’s blind spots.
After the first prototype was created, we noted a gap in the registration counter – it remained a high-touch point, was exposed to the elements, and came into direct contact with patients. We went back to the drawing board to transform registration into a contactless process to enhance protection for our staff. To enable this, we leveraged a smart scanning app designed in-house by our army engineers that automatically extracted relevant data from identity documents using optical character recognition, which improved the speed and accuracy of registration. We also figured that it was much quicker for the patients themselves to uncap and recap the specimen tubes, as the “space gloves” resulted in some degree of fine motor developmental regression.
Innovation is about doing things differently, beyond doing the same things better. Just a few decades back, we were still handing out written prescriptions and medical certificates, and house officers would spend a good hour in the morning scurrying from bed to bed to check the patient charts. Today, the electronic medical records are a godsend and it is just the beginning. Health wearables, telemedicine and data analytics are just a few of the things that are changing the healthcare landscape rapidly. It is exciting to imagine the possibilities for the kind of health technology that we might use in the near future! On the other hand, some problems do not require a technological solution, but a paradigm shift.
As my first medical innovation assignment, the MSS taught me a great deal. For those of you who have been griping about the way things are done, or are tired of hearing the words “it is what it is”, I urge you to take the first step and to get those innovation juices flowing!
Acknowledgements
I would like to thank the following individuals for their contributions to this assignment: Military Expert (ME) 6 Roy de Souza and ME4 Barry Yee from the Maintenance and Engineering Support Formation for their leadership and engineering expertise; Dr Hairil Abdullah, Dr Tan Zihui, Dr Antonia Zeng, and Dr Mavis Teo from the Singapore General Hospital Anaesthesiology Department for their input as SG-Swab Assurance For Everyone innovators and end-users; Dr Akila Andiappan and Ms Christine Fock from the Health Promotion Board for working with the SAF in scaling up the project; and COL (Dr) David Law and SLTC (Dr) Tan Nan Guang from the SAF Medical Corps for their steadfast guidance and support always.
Disclaimer
The opinions expressed in this article are the author’s personal views and do not represent those of the SAF.