Patient safety has reached its twenty year milestone since the publication of the landmark report To Err is Human in 1999 by the US Institute of Medicine. The prevalence of harm and pervasiveness of safety issues in healthcare called for attention, and efforts were dedicated to improve the reliability of healthcare systems to reduce the risk of harm to patients. The most common adverse events include hospital-acquired infections, medication errors, surgical injuries as well as safety events resulting from inadequate handoffs, pressure injuries, falls and failure to rescue.1 Advances in technology could potentially springboard innovations for patient safety with strategies to optimise care. Examples include automation of tasks, introduction of alerts and improving workforce productivity.2 This article introduces two innovative technological solutions developed locally by nurses to enhance patient safety.
A patient monitoring system for falls prevention
The prevalence of inpatient falls and related injuries poses complex challenges that impact healthcare systems worldwide, creating a heavy burden on medical and social services. In 2018, Tan Tock Seng Hospital and CoNEX Systems and Services Pte Ltd, a Singapore-based engineering solutions company, co-developed an innovative patient monitoring system named PreSAGE(r) for falls prevention in single and isolation rooms in the hospital environment. The system uses thermography, proprietary machine learning, predictive algorithms and image processing techniques to predict bed-exit situations and trigger advanced warnings to facilitate early intervention. The system was developed based on three key design principles: (i) non-contact, (ii) non-intrusive, and (iii) automated continuous monitoring.
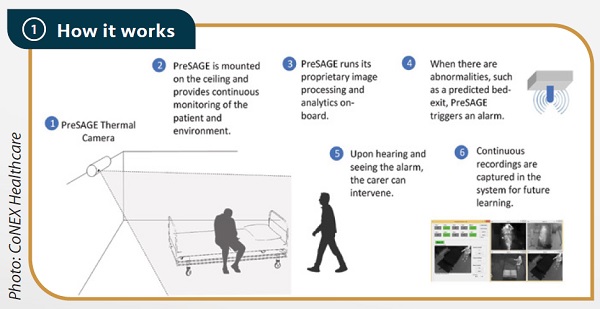
How the system works
Figure 1 illustrates how the system is operationalised in the patient care room. A thermal sensor unit is mounted on the ceiling and captures continuous movement data. Once a bed-exit behaviour is predicted, the sensor unit triggers a visual and audible alert to the nurses. When a nurse enters the room, the sensor detects a second person by the bedside and the system is momentarily deactivated. After the nurse leaves the bedside, the system switches back to monitoring mode. The automatic deactivation of the alarm when intervention is received (eg, when the nurse attends to the patient) and reactivation when risk is anticipated (eg, the patient is left alone) is a unique feature of the PreSAGE(r) system. In comparison with other bed-exit alarm detection systems, this system prevents fall incidences related to staff forgetting to re-activate the alarm system after attending to the patient. As the system uses thermography that does not capture any identifiable features of the subject, patient and staff privacy is preserved. System performance is also maintained in the absence of light, an edge over systems that use optical imaging systems for bed-exit detection.
PreSAGE(r) system set-up and operational workflow
Validation and proof-of-value demonstration
A proof-of-concept study approved by the Domain Specific Review Board was conducted with 80 recruited patients. A total of 11,573 hours of images were recorded with 223 episodes of bed-sitting positions and 93 episodes of unassisted bed-exits captured. The development of a predictive algorithm enabled an alarm trigger to allow a 15-second pre-exit lead time for staff to intervene before the patient assumes a standing position from the bed. The predictive capability of the system led to achieving a high sensitivity score of 99.7% and a specificity score of 100%. In a subsequent proof-of-value evaluation of the system in real-time ward deployment, PreSAGE(r) achieved a sensitivity score of 100% where alarms were triggered for all bed-exit attempts and a positive predictive value of 90.8%. False alarms were generated when the images of the patient and staff overlapped when staff attended to patients, resulting in auto-reactivation of the alarm system. Staff reported positive experiences with the system in a survey conducted post-deployment, including feedback on its ease of use and perceptions of improved surveillance facilitated by a live monitoring dashboard. There was a 34% reduction in falls rate and a 67% saving in manpower hours.
Bedside Alarm Recognition system
Various medical equipment and devices are used in the acute hospital for treatment or monitoring purposes. Medical equipment, including medication pumps, dialysis machines and ventilators, commonly triggers an audio alarm to signal the need for a nurse's intervention. These alarms can be both critical and time-sensitive, requiring immediate attention. In an isolation room ward configuration, sound levels emitted from the alarms are inadvertently lowered when the room doors are closed, sometimes even being inaudible from outside the patient room. This poses a safety issue when the nurse cannot be alerted in time to an equipment alarm, delaying the response to a critical situation and potentially resulting in a failure-to-rescue event. Solutions such as the use of sound amplifiers and baby monitors were assessed to be inappropriate for deployment in healthcare environments due to the need to maintain confidentiality of conversations occurring within the patient room and to ensure that patient privacy is preserved.
The Bedside Alarm Recognition (BAR) solution was co-developed with an industry partner to address the safety issue. BAR leverages on proprietary audio signal processing and machine learning techniques to enable the recognition of a range of medical equipment audio alarms while filtering human conversations and ambient noises in real time. Once the BAR device successfully recognises a medical equipment's audio alarm in the patient room, it relays the information to an external alarm indicator unit which includes both audio and visual indicators to alert the nurses for timely intervention. The BAR solution is also designed with the capability to automatically disarm when the equipment alarm is attended to and this feature enhances the ease of use and operational efficiency. Figure 2 illustrates the key benefits and features of the BAR solution.

The BAR solution's key technology features and benefits
The BAR solution is designed as a plug and play system where the device can be plugged directly into the electric wall socket in any room to facilitate rotational use of the device in different isolation rooms when needed. The BAR solution is currently in its prototype phase and will be evaluated for its performance to ensure 100% sensitivity in detecting and transmitting the alarm signals and providing a low false positive rate to prevent alarm fatigue among the nurses.
Conclusion
This article demonstrates how two innovative technological solutions developed locally by nurses could contribute significantly to patient safety. Advances in technology (eg, use of thermal sensors) can be leveraged to increase the range of digital offerings that can be creatively adapted for application in clinical settings. Nurses are aptly positioned to change practice at point of care and should continuously seek innovative ways to optimise technology for safer and better care.