On 31 December 2019, our associate consultant Dr Karrie Ko posted a Reuters report on the microbiology department junior doctors WhatsApp chat – "Chinese officials investigate cause of pneumonia outbreak in Wuhan." It didn't elicit an immediate response. At that time, most of us did not even know where Wuhan was, or that it had a population of over 11 million. It all seemed very remote.
My regular tea-buddy is from the Department of Molecular Pathology. Through January, the Wuhan pneumonia situation cropped up regularly in our discussions. If there was a need to diagnose this new disease by polymerase chain reaction (PCR), his department would bear the brunt of testing. Even back then, they were already deciding on the choice of swabs, and stockpiling reagents in anticipation of future shortages. They detected the first COVID-19 case in Singapore on 23 January 2020. At that time, I was just concluding a carefree holiday in Kyushu, Japan. My wife said that there was a noticeable change in my mood when I got the news. I could tell from my WhatsApp chats and work emails that the hospital was mobilising, as if for war.
On 6 February, my tea-buddy sent me an article reprinted in the Straits Times from Caixin Global titled "Reporter's Notebook: Life and death in a Wuhan coronavirus ICU".1 Up till then, I still harboured illusions that this could be a relatively mild illness like H1N1 in 2009; in fact, the initial cases did not seem to be as bad as SARS. However, we now know that it is precisely because many people experience mild (or no) symptoms that this virus is so successful at spreading. This article gave the first hint that if many people got infected, there would be enough very sick patients presenting in a short time to overwhelm a healthcare system.
Ramping up
Every Friday morning, the Singapore infectious diseases community meets at one of the larger public hospitals to discuss interesting cases. On 7 February, we met virtually on Zoom for the first time to discuss some of the earliest COVID-19 cases. We have not met in-person since.
The following day, the infection prevention team required all staff to wear masks in the laboratory. This seemed strange as we were not patient– fronting, and we have been handling all specimens in biosafety cabinets to reduce risk of infection since SARS in 2003. I half-joked that this was to protect us from infecting each other. I don't know if this was indeed the original intention, but in light of present universal masking guidelines, it probably was not a bad move.
The Department of Microbiology was largely spared the initial flurry of activity. However, it soon became apparent that our molecular pathology colleagues were rapidly getting swamped with work. Immediately after Lunar New Year (28 January), we decided to deploy our microbiology trainees to help them. It was an easy decision to make. This was a once-in-a-lifetime (hopefully!) opportunity for the trainees to participate in a national effort during a pandemic of historic proportions. Whatever experience they acquired would still be very relevant to their training. So far, they have assisted in the evaluation of three automated SARS-CoV-2 PCR test systems, and the validation of pooled samples and different swabs. They also assisted in data collection and statistics and reporting of SARS-CoV-2 results.
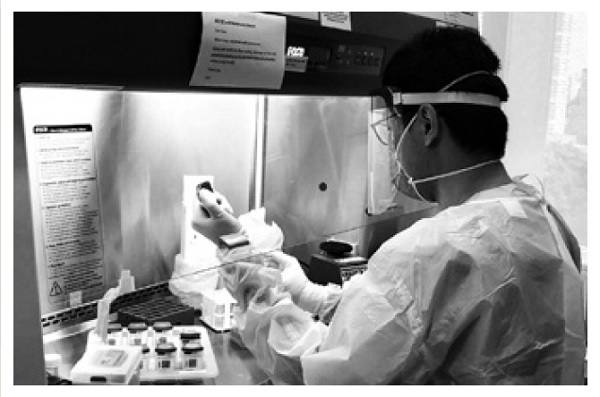 Above, Dr Kenneth Goh is seen performing an evaluation of a SARS-CoV-2 PCR test.
Above, Dr Kenneth Goh is seen performing an evaluation of a SARS-CoV-2 PCR test.
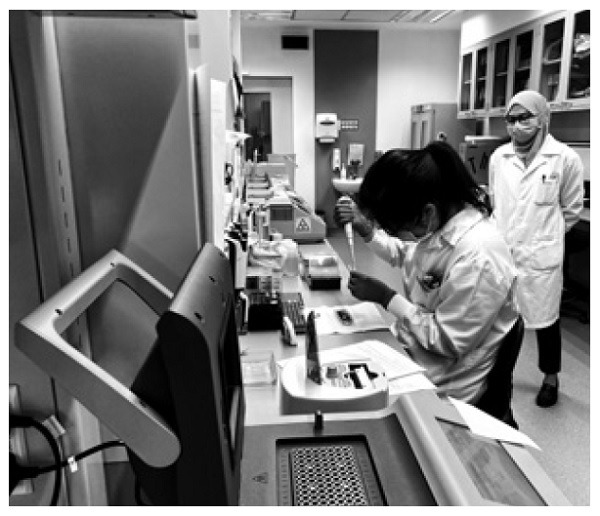
Here, Dr Deborah Lai reviews a SARS– CoV–2 PCR result in the Department of Molecular Pathology.

However, as the national demand for testing surged, this proved to be still insufficient. From 10 February onwards, up to seven microbiology medical laboratory technologists (MLT)/ medical laboratory scientists (MLS) were reassigned to molecular pathology to help with the increasing load of SARS-CoV-2 PCR requests. This was a much more painful decision, as laboratories are staffed just sufficiently to be cost-efficient during peacetime. This meant that we had to find ways of coping with less staff, and it was a scheduling nightmare for the supervisors. We even had to contemplate cutting services, though fortunately it never actually came to that.
Settling into a new routine
By April, the situation started to stabilise with the molecular pathology department having increased their staffing and capacity. We had also started introducing our own battery of COVID-19 tests.
 In the Diagnostic Bacteriology Laboratory, MLT Yap Hock Guan loads a random-access automated PCR test for SARS-CoV-2 into a machine that is also used for Methicillin-resistant Staphylococcus aureus and carbapenemase-producing Enterobacterales screening.
In the Diagnostic Bacteriology Laboratory, MLT Yap Hock Guan loads a random-access automated PCR test for SARS-CoV-2 into a machine that is also used for Methicillin-resistant Staphylococcus aureus and carbapenemase-producing Enterobacterales screening.
 Over in the Virology Laboratory, MLS Tan Chai Teng runs a high throughput COVID-19 serology test. To date, we have evaluated a total of eight different serology tests.
Over in the Virology Laboratory, MLS Tan Chai Teng runs a high throughput COVID-19 serology test. To date, we have evaluated a total of eight different serology tests.
 Under normal circumstances, the Epidemiology Laboratory carries out molecular fingerprinting of multidrug resistant bacteria for hospital outbreak investigations. Above, MLT Jolene Gien loads a sequencer under the watchful eye of senior MLS Dr Nurdyana Bte Abdul Rahman. They are sequencing SARS-CoV-2 genomes to help guide contact tracing efforts.
Under normal circumstances, the Epidemiology Laboratory carries out molecular fingerprinting of multidrug resistant bacteria for hospital outbreak investigations. Above, MLT Jolene Gien loads a sequencer under the watchful eye of senior MLS Dr Nurdyana Bte Abdul Rahman. They are sequencing SARS-CoV-2 genomes to help guide contact tracing efforts.
 Dr Karrie Ko was starting her PhD on the hospital environmental microbiome when the COVID-19 outbreak occurred. She has now redirected some of her research to the study of SARS-CoV-2 in the environment.
Dr Karrie Ko was starting her PhD on the hospital environmental microbiome when the COVID-19 outbreak occurred. She has now redirected some of her research to the study of SARS-CoV-2 in the environment.
It has been twenty-nine weeks (as of 14 July) since that initial WhatsApp post and we have settled into a kind of rhythm. We now feel naked without a mask, meetings are held via videoconference even if our offices are within walking distance from each other, and meals are consumed in solitude on-site rather than with colleagues over at Tiong Bahru Food Centre. There is a SafeEntry QR code on my office noticeboard, and we have to log in our temperature recordings twice daily. I no longer meet my tea-buddy for tea.
Despite the stress and social isolation, everybody is taking things in the right spirit and is working with a common purpose. We are painfully aware of all the suffering around the world, and are grateful to be making a direct contribution to get Singapore back on track.