Recent high-profile cases of disciplinary action against doctors have set the medical profession abuzz, causing much debate and chatter in both real-world tea rooms and virtual chat rooms, accompanied by anxiety and uncertainty over the integrity of the Singapore Medical Council's (SMC) disciplinary process and the future of the medical legal environment.
Of particular concern is the case involving "serious negligence" of a senior paediatrician who failed to diagnose a child with Kawasaki disease. The doctor was charged with professional misconduct and the Disciplinary Tribunal (DT) handed down a three-month suspension of practice. The doctor appealed but the sentence was upheld by the High Court comprising three judges. This case of a seemingly "missed diagnosis" of a rare disease caused enough consternation among doctors to start an online petition to appeal to SMC, and it eventually amassed more than 1,000 signatories (or 7.5% of the 13,000 registered doctors in Singapore), possibly the largest petition of its kind to date.
This case was also brought up in parliament on 1 August 2017, with Member of Parliament (MP) Dr Lim Wee Kiak asking if there were guidelines for doctors "to send all cases for detailed diagnostic tests to avoid misdiagnosing rare medical conditions". Another MP Ms Tin Pei Ling commented that such judgements could eventually lead to more doctors practising defensive medicine. Senior Minister of State for Health Dr Lam Pin Min replied that the practice of defensive medicine adds unnecessarily to healthcare costs, and that doctors are expected to exercise good clinical judgement and manage patients appropriately.
I fully empathise with my fellow medical colleagues and understand why this case has generated so much angst. During the course of the days and weeks of media attention on the case, emotions have run high and doctors have called for something to be done because practising medicine seems to be getting more and more difficult in an unforgiving medico-legal environment.
I strongly urge all interested doctors to read the entire Grounds of Decision of the DT and even the appeal judgement by the Court of Three Judges to fully understand the issues involved, and to come to your own conclusions. In any case, the description of Kawasaki disease contained in the appeals judgement is so detailed that it merits continuing medical education points just for the clinical update alone.
Suspension being too harsh
Many people believed that the punishment of a three-month suspension was too harsh, as suspension from practice is something that should be reserved for the most serious of negligence cases, such as wilful misconduct and bringing the profession into disrepute. Most of us have no issue with past cases of suspension for doctors who overprescribe addictive drugs or engage in fraudulent activity, for example.
Being suspended leaves a permanent record on a doctor's performance and will affect the doctor's future prospect of finding employment or working abroad where a certificate of good standing would be required.
In this case, the suspension was seemingly meted out in a situation of cognitive error, a missed diagnosis of a rare illness and the making of a wrong clinical decision. The DT saw it differently and dealt with it as a case of serious negligence where the doctor had failed to follow international guidelines to act to run confirmatory tests on a number of occasions, even after the diagnosis of Kawasaki disease was considered. One of the main points of the petition to the Ministry of Health (MOH) was that the signatories felt that a censure or warning, instead of a three-month suspension, would have been more appropriate.
Cognitive error versus serious negligence
It is hard to define what constitutes serious negligence, as it depends on the context of the case, the qualifications and experience of the doctor, and the opinions of the expert witness.
It is worthwhile to note the comments of the High Court in Chia Foong Lin:
"[60] In Low Cze Hong, the court stated at [32] that "misconduct" means "more than mere negligence". It added that "[g]ross negligence might amount to relevant misconduct, particularly if accompanied by indifference to, or lack of concern for, the welfare of the patient." Mere errors of judgment and professional incompetence are insufficient to lead to a finding of gross negligence."
"[61] ...While we recognise that the line between an error of judgment and gross negligence could in certain circumstances be fine and that an error of judgment does not, ipso facto, constitute professional misconduct, it is the entire picture which will be determinative."
As can be seen, it is not easy to describe or define when an "honest mistake" or cognitive error becomes serious negligence. It is a matter of degree. A simple mistake may be an error of judgement, but repeated lapses of behaviour that show no concern for patient welfare may then become a case of serious negligence. Where the line was crossed is a judgement call made by the DT and based on context. Clinical intuition is used to make snap decisions in real life, whereas deliberate decision-making is harder as it requires the doctor to follow clinical protocols and memorise decision pathways. In order to reduce cognitive error, the logical consequence is to discourage intuition and lean towards more protocol-driven practices, with defensive medicine being one of the possible undesired outcomes.
Self-regulation
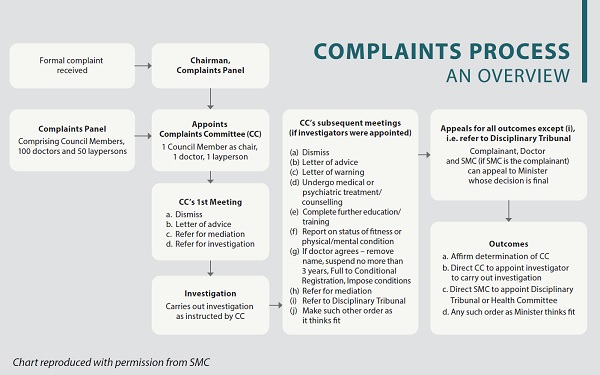
Doctors have also expressed unhappiness that once found guilty of serious negligence, suspension is therefore "required" and the minimum period as set out in the Medical Registration Act (MRA) is three months. The system does not seem to differentiate between first-time and repeat offenders, although a past history of good clinical practice is given some weight during the tribunal deliberations. Should the process allow for more leniency in cases where there was no malicious intent, no act of harm, or in cases where the complaint has no merit? I have even heard comments inferring that sentencing was somehow "dished out" by SMC or that SMC is able to influence and set the tone of the punishment, which is clearly misguided. The answers to some of these questions reside in having a good understanding of the entire disciplinary process, which I have set out in a separate box (see page 11).
I have previously served on a few complaints committees (CC) and can attest to the dedication of those appointed on the panel to ensure that complaints brought to SMC had merit, that the doctor was given a fair chance to provide his or her explanation, and to ensure that patients were protected, standards were upheld and justice was served.
Between 2012 and 2016, there was an average of 176 complaints per year. On average, the CC dismissed 88 cases, issued letters of advice to 41 cases, and issued letters of warning to nine cases. Only about 16 cases, on average, were referred to the DT per year, slightly less than 10% of complaints. This shows that the CC is able to exercise independent judgement and discretion in the cases that it handles.
Between 2012 and 2016, there were a total of 69 cases handled by the DT, of which eight were discontinued/withdrawn, five resulted in acquittals, one resulted in a restriction of practice, one case of censure, 16 cases of censures plus fine, 23 cases of suspension, and three doctors were removed from the register.1
As only one third of cases referred to the DT resulted in suspension, being called to a DT therefore does not mean automatic suspension, but it does mean that the case was considered serious enough to be referred by fellow peers sitting in the CC.
The point in understanding the disciplinary process is that it underscores the importance of professional self-regulation. It should always be the case that doctors are judged by their peers, because only fellow medical practitioners are able to appreciate the varied levels of context and nuances in clinical practice. However, with increasing patient knowledge and emphasis on autonomy, it is becoming harder to justify self-regulation in the face of scepticism that such a system is maintained to protect doctors. Therefore, as a medical profession, we must work together to ensure a robust and fair disciplinary process that reinforces trust.
Improving the system
Amending the MRA
The minimum suspension period of three months is specified in the MRA (see Disciplinary Process on page 11), which could be amended to allow for more leeway in sentencing. There have been cases that did not warrant such a harsh sentence; even the High Court acknowledged this in Eu Kong Weng:
"[7] We agree that a suspension is called for, and if we had the discretion, we would have imposed a shorter period of suspension. However, the law does not allow us to do that as the 3-month suspension is the minimum mandated by s 45(2)(b) of the Act."
Changing the law will be a slow process as any proposed amendment would have to be reviewed by SMC and submitted to the Ministry of Health for further review. Following which, consultations with external bodies, such as the Ministry of Law, the Attorney-General's Chambers and the public, must take place before the changes are tabled in Parliament.
Complaints Panel
The MRA provides for 100 doctors on the SMC Complaints Panel who are appointed over a two-year term. For each two-year appointment, SMC would approach public and private hospitals and medical institutions, as well as the professional bodies (eg, Academy of Medicine Singapore [AMS], College of Family Physicians Singapore [CFPS], SMA) to submit their nominations of doctors from various specialties to be considered for appointment to the Panel.
Doctors with at least ten years' standing can volunteer to be on the Complaints Panel, bearing in mind that they are there to set the standards that all doctors have to prescribe to. Doctors who serve on the CC will also benefit from the experience and develop better awareness of medico-legal pitfalls that should be avoided. The number of doctors allowed on the panel should be increased to reflect the growth in numbers of registered doctors in Singapore.
Expert witnesses
We need more expert witnesses to serve in the disciplinary proceedings. An expert witness is one who is able to articulate the standard of care and professional conduct expected of doctors, and to give impartial and objective opinions to assist the court. The expert witness acts independently and technically does not owe any obligation to the party who engages his expertise. The problem is that we only have a small pool of doctors who are willing to be expert witnesses and come forward to spend time and contribute to the legal proceedings. We should not be quick to criticise these fellow colleagues whose opinions may result in judgements that we disagree with.
On this last note, I would encourage all interested doctors to consider signing up for the Medical Expert Witness Training programme. This is a joint collaboration between AMS, Law Society of Singapore, Singapore Academy of Law, SMA and the State Courts of Singapore. Participants are taught how to write good expert reports, and also given a chance to role play in court rooms and have a go at the "hot seat" to give evidence in mock trials. The faculty comprises trainers who are district judges, lawyers and senior doctors. In the most recent course held over three weekends from June to July 2017, ten judges and 16 lawyers participated. This was the third instalment of the programme and since then, we have equipped more than 100 doctors with the skills to be expert witnesses.
In the future, we hope to have a large pool of expert witnesses to tap on. Academic bodies such as AMS and CFPS can also be approached to provide assistance in recommending appropriate expert witnesses. Such active engagement of healthcare stakeholders would help contribute to more trust and ownership of the disciplinary process in Singapore.
The disciplinary process
The disciplinary process is specified in the MRA and its objectives are to protect the health and safety of the public, uphold standards of practice within the medical profession, and maintain public confidence in the medical profession. The MRA provides two types of disciplinary bodies – the CC and the DT, whose proceedings, deliberations and decisions are entirely independent of the SMC.
It is important to understand that the majority of complaints do not make its way to a DT. As a first cut, aggrieved patients who approach SMC are screened and advised on whether their complaints bear merit. The SMC information sheet2 that is available online makes it clear that SMC will only consider complaints made against doctors, and is not empowered to investigate complaints that pertain to institutional policies, such as appointment scheduling and billing. The SMC does not deal with requests for refunds, compensations, retrieval of medical records, and the seeking of apologies from doctors. The SMC secretariat members who deal with complaints as a first point of contact will also see if such cases can be resolved through facilitating communication with the institution or the doctor concerned, or through mediation. Cases that are deemed able to proceed will require a signed statutory declaration by the patient addressed to chairman of the SMC CC.
The Complaints Committee
The Complaints chairman then appoints a CC comprising one SMC council member as chair, one registered doctor of at least ten years' standing, and one lay member. There are about 100 doctors and 50 laypersons who volunteer their time to be part of the panel in the CC. At the first CC meeting, clear cut cases with no merit and those that are deemed "frivolous, vexatious, misconceived or lacking in substance" can be dismissed. If need be, doctors who have fallen short of expected standards will be issued a letter of advice or letter of warning, or have their cases referred for mediation. In more serious or complex cases, the CC can instruct that further investigations be made or opinions sought from an expert witness before they decide to refer to the DT.
The Disciplinary Tribunal
The chairman of the DT can be a senior doctor, senior lawyer, ex-judge or ex-judicial commissioner. The chairman is advised by doctors selected from the CC. The CC members are not allowed to sit in the DT for the same case.
The powers of the DT include removing the doctor from the register, suspending the doctor for "not less than 3 months and not more than 3 years", imposing a fine not exceeding $100,000, handing out a censure or letter of undertaking, or make such other order as DT thinks fit. The doctor can appeal the decision at the High Court, also known as the Court of Three Judges, whose decision is final. SMC or MOH do not have any legal recourse to review a case after it has gone through the court of appeal.
MRA amendments
You might recall that the current MRA was amended in 2010, granting more powers to the CC, including the referral of cases for mediation between the doctor and the patient. That was also the time when changes were introduced to the composition of DTs with the inclusion of senior lawyers and retired judges to chair the DT. SMA gave feedback to SMC during the MRA consultation in 2009, recommending that the DT chairperson should be an SMC council member (a registered doctor) instead of a lawyer or retired judge.
In their press release published in October 2012, the SMC president explained that this was to "significantly improve the quality and pace of the proceedings before the Disciplinary Tribunals, particularly in dealing with legal issues that may arise, while preserving the fundamental principle of self-regulation."3
Following this, in January 2013, the then Director of Medical Services wrote in a letter4 addressed to doctors that "the DT would still be constituted with a majority of doctors so that questions of fact relating to medical issues are fully and justly considered. The legal person appointed to chair would not have a casting vote in the event of a tie and the views of the majority of doctors on the DT would prevail. To a large extent, the Chair's role would be to manage the conduct of the hearing."
