Perimenopause is a natural transition that all women go through, marking the period leading up to menopause. During early perimenopause, menstrual cycles become irregular, with fluctuations of more than seven days between consecutive cycles. In late perimenopause, women may miss their periods for over two months. The menopause transition usually lasts for one to three years. Menopause is clinically defined as the absence of menstruation for over a year, typically in women over the age of 45. For women under the age of 45 or those with atypical symptoms, testing for follicle-stimulating hormone levels can help confirm menopause onset.
Menopause occurs when one's ovaries exhaust their egg supply, leading to a decrease in oestrogen and progesterone levels, which in turn causes menstrual cessation. Oestrogen receptors are located throughout the body and affect multiple organ systems, so menopausal symptoms vary widely among individuals.
Symptoms of menopause
Menopausal symptoms usually begin during perimenopause and can last for years after menopause. They include irregular menstrual cycles, sleep disturbances, and vasomotor, cognitive, musculoskeletal and genitourinary symptoms.
Vasomotor symptoms
The most classic menopause symptoms are vasomotor symptoms (VMS), which include hot flushes and night sweats. Hot flushes are characterised by intense heat in the upper body lasting for one to five minutes, sometimes accompanied by sweating, chills, anxiety and heart palpitations. Night sweats, which are hot flushes that occur during sleep, can also occur. Around 80% of women experience hot flushes during menopause, with 25% reporting severe and debilitating symptoms. The median duration of these symptoms is seven years. VMS can disrupt sleep, mood, concentration, energy, leisure, work, social activities and sexual health.
Lifestyle interventions, such as weight loss for overweight or obese women, have been shown to improve VMS. Menopausal hormone therapy (MHT) is the first-line treatment for VMS in most women, provided there are no contraindications such as oestrogen-dependent cancers or a history of cardiovascular disease (CVD) or venous thromboembolism (VTE). For those who cannot or choose not to use MHT, alternative treatments like selective serotonin reuptake inhibitors, gabapentin, and the recently US Food and Drug Administration-approved fezolinetant (targeting the thermoregulatory centre in the brain) may offer relief. Cognitive behavioural therapy, either self-guided or in therapy sessions, may also be beneficial. There is no strong evidence supporting the effectiveness of herbal supplements like evening primrose oil, black cohosh or red clover in alleviating VMS.
Sleep disturbances
Women in perimenopause commonly experience sleep disturbances due to hormonal changes, hot flushes and mood swings. It is crucial to rule out sleep disorders like sleep apnoea or restless leg syndrome. Lifestyle changes can help, such as establishing a regular sleep schedule, creating a relaxing bedtime routine (eg, reading or meditation), optimising the sleep environment to be cool, dark and quiet, limiting caffeine and alcohol intake, and engaging in regular physical activity. However, strenuous exercise should be avoided near bedtime.
Cognitive symptoms
Cognitive difficulties, often described as brain fog, are commonly reported during perimenopause. Women in perimenopause frequently experience issues with concentration, memory lapses and forgetfulness. Research confirms that menopause can temporarily affect cognitive function, but these changes are typically mild and tend to improve post-menopause. It is important to reassure women that menopause-related cognitive changes are not indicative of early-onset dementia. Maintaining cardiovascular health through a balanced diet and regular exercise, engaging in cognitively stimulating activities, and fostering social connections can support brain health during this transition.
Musculoskeletal symptoms
Declining oestrogen levels can also contribute to musculoskeletal symptoms, including joint pain, muscle loss and reduced bone density, a condition now referred to as the musculoskeletal syndrome of menopause. To mitigate these effects, women should be encouraged to maintain adequate calcium, vitamin D and protein intake, along with engaging in resistance training and weight-bearing exercises to preserve muscle mass and bone strength.
Genitourinary symptoms
The genitourinary syndrome of menopause (GSM) encompasses vaginal dryness, sexual discomfort and urinary symptoms like urinary urgency, dysuria and recurrent urinary tract infections. Lifestyle advice includes proper perineal hygiene and the use of vaginal moisturisers for mild symptoms. Vaginal oestrogen (administered by cream, tablet or ring) is the most effective treatment for GSM, helping restore vaginal moisture, thickness and pH balance. Low-dose vaginal oestrogen has minimal systemic absorption and no increased risk for breast cancer, stroke or deep vein thrombosis, making it safe for long-term use.
Long-term health consequences
Even in the absence of severe symptoms, menopause brings significant long- term health implications, including changes in cardiometabolic health and bone density. Many women experience weight gain during perimenopause, with fat redistribution favouring the abdominal area. This shift is associated with an increased risk of insulin resistance, dyslipidaemia and CVD. Studies have also linked the severity of VMS to a heightened risk of CVD. Therefore, midlife women should be advised to monitor cardiovascular risk factors such as obesity, hypertension and diabetes, with appropriate lifestyle modifications and medical interventions as needed.
Bone health is another critical concern, as oestrogen deficiency accelerates bone loss, increasing the risk of osteopenia and osteoporosis. Women at higher risk – such as those with premature menopause, low body weight, a family history of osteoporosis or fractures, or medical conditions that contribute to bone loss – should undergo bone mineral density screening. MHT has been shown to be effective in preventing bone loss and reducing the risk of fragility fractures.
Menopausal hormone therapy
MHT usage experienced a decline following a 2002 Women's Health Initiative study due to concerns about breast cancer and CVD risks. However, later analyses have shown more favourable outcomes in women who start MHT closer to the onset of menopause. MHT is generally considered safe for women under the age of 60 or those within ten years of menopause onset, provided that there are no contraindications.
MHT is indicated for managing VMS, treating urogenital atrophy, addressing premature menopause (before age 45), and preventing osteoporosis in high-risk individuals. It may also alleviate symptoms like joint and muscle pain, mood swings, sleep disturbances and sexual dysfunction. However, MHT should not be used as a preventive measure for CVD or dementia for women who undergo menopause at the usual age. Treatment should be individualised, taking into account the woman's symptoms, quality of life, health risks, age and personal preferences. Women on MHT should have annual consultations to assess their health status and discuss whether to continue or adjust treatment.
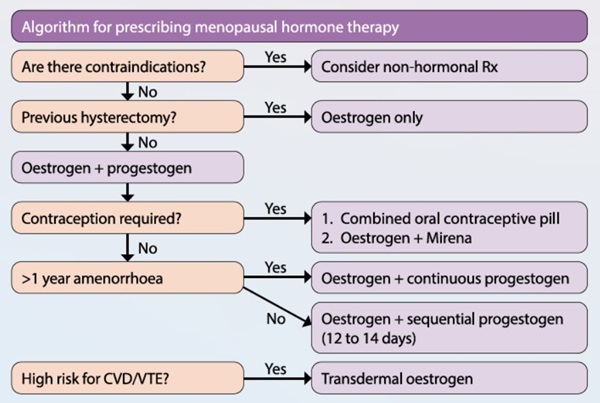
Oestrogen therapy is suitable for women who have undergone a hysterectomy, while oestrogen and progestogen therapy is recommended for women who still have their uterus to protect against endometrial hyperplasia and cancer, which can occur with unopposed oestrogen therapy. Sequential MHT is usually given to perimenopausal women while continuous MHT is given to postmenopausal women. Transdermal oestrogen can be considered for women who are at higher risk of CVD or VTE (eg, those with body mass index >30 kg/m2, diabetes, hypertriglyceridemia or migraines). Generally, it is safe to stop contraception in women under the age of 50 years after two years of amenorrhoea or in women over the age of 50 years after one year of amenorrhoea.
Conclusion
Perimenopause and menopause are natural, inevitable transitions in a woman's life, but they bring with them various challenges, both physical and psychological. By understanding the symptoms and available treatments, healthcare providers can offer targeted support to help women manage this phase of life. Lifestyle modifications, including dietary changes, physical activity and mental health support, are essential components of care. For women experiencing moderate-to-severe symptoms, MHT can be an effective treatment, though it requires careful consideration and ongoing monitoring. With the right interventions and education, women can navigate menopause with improved quality of life and reduced long-term health risks.